How to Properly Clean Medical Devices
Tweet
 Print
Print
When it comes to medical devices cleanliness is crucial. All medical devices, whether they are disposable, implantable or reusable, must be cleaned during the manufacturing process to remove oil, grease, fingerprints and other manufacturing soils. Reusable products must also be thoroughly cleaned and sterilized between each use to avoid infecting patients or causing illness. Reaching the right level of cleanliness does not come automatically. A well planned cleaning regimen must be developed and followed carefully.

Developing a Cleaning Process
Medical device manufacturers must provide proof that their products can be adequately cleaned as part of the FDA approval process. As a result, most manufacturers now incorporate setting up a cleaning protocol as part of the design and development phase.
Factors to consider when setting up a cleaning regimen:
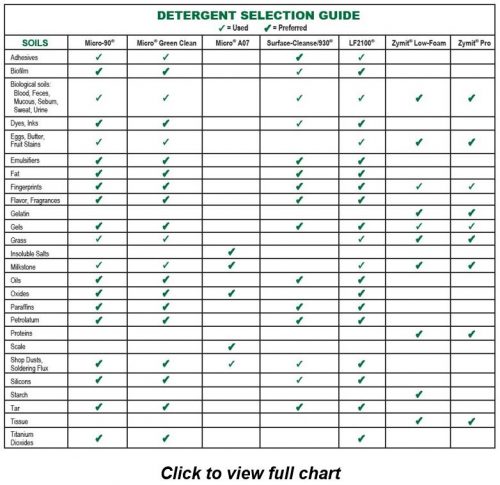
- Soils: Choose a cleaner that will best attack the soils you are trying to remove. Enzyme cleaners are often used for medical device cleaning applications since they work well at removing organic soils. Protease enzymes in particular are a good choice for protein based organic soils like blood, fat, sweat, mucous, feces and tissue.
- Surface: Titanium, plastic, ceramic, silicone and metal are some of the more common materials used in the manufacture of medical devices. It’s important to select a cleaner that is compatible with the substrate of the device you are cleaning. The cleaner manufacturer should be able to guide you and provide compatibility studies for their products.
- Wash method: Common methods of cleaning medical devices include automatic washers, ultrasonic cleaners and manual washing. Factors such as soil, substrate, composition and end use of the device are taken into consideration. Regardless of the method used, it’s extremely important to be sure that all soils are removed from blind holes and internal passages of the device.
- Temperature: In most cases, increasing the temperature is one of the best ways to speed up or improve the cleaning action. The temperature parameters that should be used for any individual cleaning application will depend upon the make-up of the medical device and the soils that are present, as well as your choice of detergent and wash method. Check with the manufacturer for the maximum suggested operating temperature for your detergent.
- Dwell time: The length of the cleaning cycle contributes to the effectiveness of your cleaning application. In most cases, a longer dwell time will improve the results. However, all factors – soils, temperature, substrate, detergent and cleaning method must be taken into consideration.
- Rinse step: Thorough rinsing should follow cleaning. Rinsing removes any excess detergent left on the item. For critical cleaning applications it is best to use deionized or distilled water, as rinsing with ordinary water may introduce new contaminates.
- Validation procedures: Cleaning validation is a part of the regulatory compliance process for medical device manufacturing and reprocessing. Validation ensures that medical devices are washed according to previously determined standards and that all traces of soil and detergent are removed. Validation methods are unique to each detergent and should be available from most cleaner manufacturers.
Download IPC’s “7 Step Guide to the Proper Usage of Critical Cleaners” for more information on establishing a cleaning regimen.
Cleaning and Sterilizing
What’s the Difference?
Medical devices not only need to be clean, they also need to be sterile. Medical devices that are not properly cleaned and sterilized can lead to patient infection. Cleaning and sterilization are two distinct processes and both must be performed to ensure that medical devices meet safety standards.
The CDC defines cleaning as “the removal of foreign material (e.g., soil, and organic material) from objects…normally accomplished using water with detergents or enzymatic products”. (https://www.cdc.gov/infectioncontrol/guidelines/disinfection/cleaning.html). They describe sterilization as a process that “destroys all microorganisms on the surface of an article or in a fluid to prevent disease transmission associated with the use of that item”. (https://www.cdc.gov/infectioncontrol/guidelines/disinfection/sterilization/index.html). The CDC has established guidelines that are used to determine if a medical device is considered sterile. This is referred to as the sterility assurance level or SAL of a product and is defined as the likelihood that any viable microorganisms will exist on a device after sterilizing.
Why do Both?
Clearly we have two different, albeit related, processes. So, why do both? Cleaning the medical devices first ensures that they are free from soils and debris that can cause infection and reduce the efficiency of the sterilization process.
The CDC guidelines explain that “Thorough cleaning is required before high-level disinfection and sterilization because inorganic and organic materials that remain on the surfaces of instruments interfere with the effectiveness of these processes. Also, if soiled materials dry or bake onto the instruments, the removal process becomes more difficult and the disinfection or sterilization process less effective or ineffective.” (https://www.cdc.gov/infectioncontrol/guidelines/disinfection/cleaning.html).
If a surface is sterilized or disinfected before it is cleaned, the remaining soils can still contribute to the growth of harmful germs and lead to further contamination. Lingering soils on the surface of the medical device can serve as a barrier and impact the efficiency of the sterilization process. If the surface is thoroughly cleaned first, and validated for cleanliness, sterilization is much more effective.
Interested in learning more about choosing the right specialty cleaner for your medical device cleaning application? Contact one of International Products Corporation’s (IPC) technical specialists or request a free cleaner sample for testing. All of IPC’s specialty cleaners are registered with NSF as A1 cleaners and can be validated in FDA processes.

Tweet
 Print
Print